Hearing Loss. Save
Hearing is a gift.hearing is the ability to be able to listen to the external sounds. Hearing loss or hearing impairment is the reduced ability to listen to external sounds.…
Listing out the pathology notes for the MBBS students. this note is about the Important bodies in pathology in various diseases and conditions::
Hearing is a gift.hearing is the ability to be able to listen to the external sounds. Hearing loss or hearing impairment is the reduced ability to listen to external sounds.…
The test gives a score, known as a Recurrence Score, from 0 to 100.
The higher the score, the more likely breast cancer is to come back and the more likely you are to benefit from having chemotherapy as well as hormone therapy.
Your specialist will use the score, along with other information about your breast cancer, to help decide whether chemotherapy would benefit you.5…
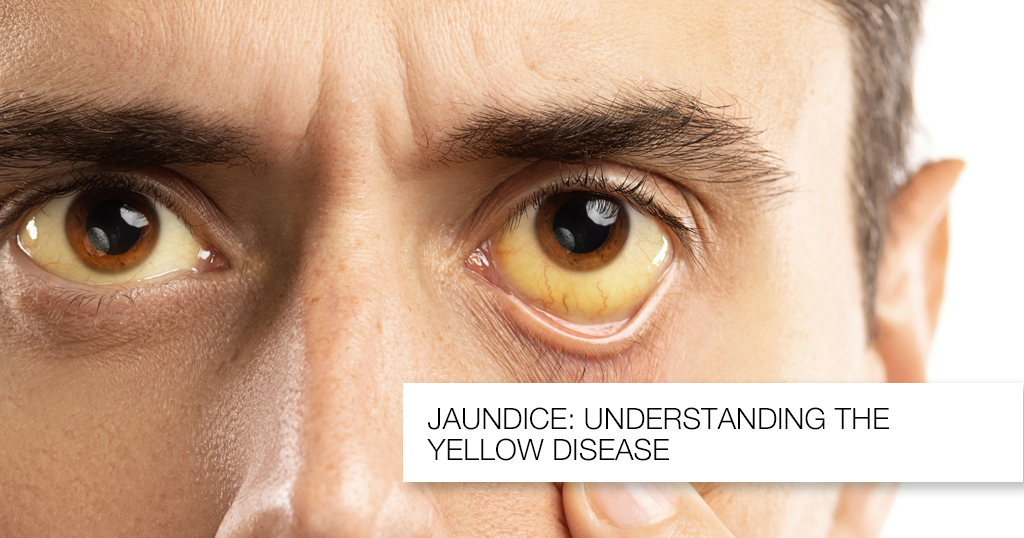
Jaundice aundice results from high levels of bilirubin in the blood. Bilirubin is the normal breakdown product from the catabolism of haem, and thus is formed from the destruction of red blood cells. Under normal…
Guidelines for the perioperative administration of fluid
are often based on static hemodynamic targets such as
central venous pressure, and delayed volume status
indexes such as blood pressure, heart rate, capillary
refill, and urine output. Traditional fluid management
protocols also rely heavily on algorithmic estimates
of fluid deficit, intravascular fluid volume status, fluid
loss, and basal fluid requirements to guide perioperative
fluid administration. Such formulaic approaches
lack definitive physiologic endpoints for determining
fluid optimization and fail to address the roles of tissue
oxygenation and end-organ perfusion in achieving
positive long-term patient outcomes. Recent advances
in hemodynamic monitoring have produced sophisticated
dynamic measures of volume status, such as
stroke volume variation and pulse pressure variation,
which may serve as functional indexes for perioperative
fluid administration.
This article reviews randomized controlled trials measuring
the impact of perioperative goal-directed therapy
on outcomes among patients undergoing high-risk
surgical procedures. A broad literature search was conducted,
and 12 studies met the inclusion criteria. Studies
were evaluated for design, population, goal-directed
therapy targets, monitoring devices used, clinical endpoints,
methods, and results. Goal-directed therapy was
associated with decreased hospital stay compared with
the control group (in 7 studies) and reduced number of
postoperative complications (7 studies).
Keywords: Fluid management, goal-directed therapy,
hemodynamic monitoring, optimization, perioperative.
REFERENCES
1. Bundgaard-Nielsen M, Holte K, Secher NH, Kehlet H. Monitoring of perioperative
fluid administration by individualized goal-directed therapy.
Acta Anaesthesiol Scand. 2007;51(3):331-340.
2. Brandstrup B. Fluid therapy for the surgical patient. Best Pract Res Clin
Anaesthesiol. 2006;20(2):265-283.
3. Lees N, Hamilton M, Rhodes A. Clinical review: goal-directed therapy
in high risk surgical patients. Crit Care. 2009;13(5):231. http://ccforum.
com/content/pdf/cc8039.pdf. Accessed May 03, 2012.
4. Rivers E, Nguyen B, Havstad S, et al; Early Goal-Directed Therapy Collaborative
Group. Early goal-directed therapy in the treatment of severe sepsis
and septic shock. N Engl J Med. 2001;345(19):1368-1377.
5. Gan TJ, Soppitt A, Maroof M, et al. Goal-directed intraoperative fluid
administration reduces length of hospital stay after major surgery. Anesthesiology.
2002;97(4):820-826.
6. Donati A, Loggi S, Preiser JC, et al. Goal-directed intraoperative therapy
reduces morbidity and length of hospital stay in high-risk surgical
patients. Chest. 2007;132(6):1817-1824.
7. West S, King V, Carey TS, et al. Systems to Rate the Strength of Scientific
Evidence. Rockville, MD: Agency for Healthcare Research and Quality;
2002. AHRQ publication 02-E016.
8. Young JM, Solomon MJ. Improving the evidence base in surgery: sources
of bias in surgical studies. ANZ J Surg. 2003;73(7):504-506.
9. Viera AJ, Bangdiwala SI. Eliminating bias in randomized controlled
trials: importance of allocation concealment and masking. Fam Med.
2007;39(2):132-137.
368 AANA Journal October 2013 Vol. 81, No. 5 www.aana.com/aanajournalonline
10. Stanley K. Evaluation of randomized controlled trials. Circulation.
2007;115(13):1819-1822.
11. Schünemann HJ, Best D, Vist G, Oxman AD, GRADE Working Group.
Letters, numbers, symbols, and words: how to communicate grades of
evidence and recommendations. CMAJ. 2003;169(7):677-680.
12. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports
of randomized clinical trials: is blinding necessary? Control Clin Trials.
1996;17(1):1-12.
13. Centre for Evidence-based Medicine Levels of Evidence Working
Group. The Oxford 2011 levels of evidence. http://www.cebm.net/
index.aspx?o=5653. Accessed September 10, 2012.
14. Guyatt GH, Oxman AD, Kunz R, et al; GRADE Working Group. Going
from evidence to recommendations [published correction appears in
BMJ 2008;336(7658):0]. BMJ. 2008;336(7652):1049-1051.
15. Shoemaker WC, Appel PL, Kram HB, Waxman K, Lee TS. Prospective
trial of supranormal values of survivors as therapeutic goals in highrisk
surgical patients. Chest. 1988;94(6):1176-1186.
16. Gattinoni L, Brazzi L, Pelosi P, et al. A trial of goal-oriented hemodynamic
therapy in critically ill patients: SvO2 Collaborative Group. N
Engl J Med. 1995;333(16):1025-1032.
17. Desborough JP. The stress response to trauma and surgery. Br J
Anaesth. 2000;85(1):109-117.
18. Hill AG. Initiators and propagators of the metabolic response to
injury. World J Surg. 2000;24(6):624-629.
19. Sandham JD, Hull RD, Brant RF, et al; Canadian Critical Care
Clinical Trials Group. A randomized, controlled trial of the use of
pulmonary-artery catheters in high-risk surgical patients. N Eng J Med.
2003;348(1):5-14.
20. Atlas GA, inventor; Licata and Tyrrell, assignee. Modified esophageal
Doppler monitor methods for measuring aortic DP/DT and pulse
wave velocity. US patent 2005/0187468A1. August 25, 2005.
21. Wakeling HG, McFall MR, Jenkins CS. Intraoperative oesophageal
Doppler guided fluid management shortens postoperative hospital
stay after major bowel surgery. Br J Anaesth. 2005;95(5):634-642.
22. Noblett SE, Snowden CP, Shenton BK, Horgan AF. Randomized
clinical trial assessing the effect of Doppler-optimized fluid management
on outcome after elective colorectal resection. Br J Surg.
2006;93(9):1069-1076.
23. Cecconi M, Fasano N, Langiano N, et al. Goal-directed haemodynamic
therapy during elective total hip arthroplasty during regional
anesthesia. Crit Care. 2011;15(3):R132. http://ccforum.com/content/
pdf/cc10246.pdf. Accessed April 30, 2012.
24. Buettner M, Schummer W, Huettemann E, Schenke S, van Hout N,
Sakka SG. Influence of systolic-pressure-variation-guided intraoperative
fluid management on organ function and oxygen transport. Br J
Anaesth. 2008;101(2):194-199.
25. Jammer I, Ulvik A, Erichsen C, Lodemel O, Ostgaard G. Does central
venous oxygen saturation-directed fluid therapy affect postoperative
morbidity after colorectal surgery? A randomized assessor-blinded
controlled trial. Anesthesiology. 2010;113(5):1072-1080.
26. Forget P, Lois F, de Kock M. Goal-directed fluid management based on
the pulse oximeter-derived pleth variability index reduces lactate levels
and improves fluid management. Anesth Analg. 2010;111(94):910-914.
27. Challand C, Struthers R, Sneyd JR, et al. Randomized controlled trial of
intraoperative goal-directed therapy in aerobically fit and unfit patients
having major colorectal surgery. Br J Anaesth. 2012;108(1):53-62.
28. Strunden MS, Heckel K, Goetz AE, Reuter DA. Perioperative fluid and
volume management: physiological basis, tools, and strategies. Ann
Intensive Care. 2011;1(1):2. http://www.annalsofintensivecare.com/
content/pdf/2110-5820-1-2.pdf. Accessed April 30, 2012.
29. Benes J, Chytra I, Altmann P, et al. Intraoperative fluid optimization
using stroke volume variation in high risk surgical patients: results of
prospective randomized study. Crit Care. 2010;14(3):R118. http://
ccforum.com/content/pdf/cc9070.pdf. Accessed April 27, 2012.
30. FloTrac system [product brochure]. Irvine, CA: Edwards Lifesciences
LLC; 2007. http://ht.edwards.com/resourcegallery/products/mininvasive/
pdfs/ar02456.pdf. Accessed May 20, 2012.
31. Edwards Lifesciences LLC. Normal hemodynamic parameters and
laboratory values [pocket card]. Irvine, CA: Edwards Lifesciences
LLC; 2009. http://ht.edwards.com/scin/edwards/sitecollectionimages/
edwards/products/presep/ar05688_parameters.pdf Accessed July 29,
2013.
32. PiCCO-technology: normal values. Munich, Germany: PULSION
Medical Systems; 2008. http://www.pulsion.com/fileadmin/pulsion_
share/Products_Flyer/PiCCO_decisiontree_EN_PC81607_
R08_131008.pdf. Accessed September 4, 2012.
33. Lobo SM, Salgado PF, Castillo VG, et al. Effects of maximizing oxygen
delivery on morbidity and mortality in high-risk surgical patients. Crit
Care Med. 2000;28(10):3396-3404.
34. Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED.
Early goal-directed therapy after major surgery reduces complications
and duration of hospital stay: a randomised, controlled trial
[ISRCTN38797445]. Crit Care. 2005;9(6):R687-693. http://ccforum.
com/content/pdf/cc3887.pdf. Accessed May 18, 2012.
35. Lopes MR, Oliveira MA, Pereira VO, Lemos IP, Auler JO Jr, Michard
F. Goal-directed fluid management based on pulse pressure variation
monitoring during high-risk surgery: a pilot randomized controlled
trial. Crit Care. 2007;11(5):R100. http://ccforum.com/content/pdf/
cc6117.pdf. Accessed May 01, 2012.
36. Mayer J, Boldt J, Mengistu AM, Rohm KD, Suttner S. Goal-directed
intraoperative therapy based on autocalibrated arterial pressure
waveform analysis reduces hospital stay in high risk surgical patients:
a randomized controlled trial. Crit Care. 2010;14(1):R18. http://ccforum.
com/content/pdf/cc8875.pdf. Accessed May 03, 2012.
37. LiDCO plus [product brochure]. Cambridge, UK: LiDCO Cardiac
Sensor Systems; 2009. http://www.lidco.com/archives/LiDCOplus_
brochure_1914.pdf. Accessed August 30, 2013.
38. PiCCO plus [product brochure]. Munich, Germany: PULSION Medical
Systems; 2007. http://www.pulsion.de/fileadmin/pulsion_share/
Products/PiCCO/US/PiCCOplus_ShortSetup_US_MPI812905US_
R00_190407.pdf. Accessed May 31, 2012.
39. Walley KR. Use of central venous oxygen saturation to guide therapy.
Am J Respir Crit Care Med. 2011;184(5):514-520.
40. Bronicki RA. Venous oximetry and the assessment of oxygen transport
balance. Pediatr Crit Care Med. 2011;12(4 suppl):S21-S26.
41. Zaja J. Venous oximetry. Signa Vitae. 2007;2(1):6-10.
42. CardioQ-ODM Oesophageal Doppler Monitor: NICE Medical Technology
Guidance 3. London, UK: National Institute for Health and
Clinical Excellence; March 2011. http://www.nice.org.uk/nicemedia/
live/13312/52624/52624.pdf. Accessed June 23, 2012.
AUTHORS
Crystal D. Trinooson, CRNA, MS, is a staff nurse anesthetist at Keck Medical
Center of the University of Southern California (USC). She received
her master of science in nurse anesthesiology from the Keck School of
Medicine of USC, Program of Nurse Anesthesia.
Michele E. Gold, CRNA, PhD, is the program director and associate
professor of clinical anesthesiology at Keck School of Medicine of USC,
Program of Nurse Anesthesia.