Oncotype DX
1. What is the Oncotype DX test?
2. Who is Oncotype DX for?
3. Why is it used?
4. How does it work?
5. Oncotype DX score
6. Availability and cost
7. Oncotype DX Breast DCIS Score test
1. What is the Oncotype DX test?
Oncotype DX is a test that predicts how likely breast cancer is to spread to somewhere else in the body (secondary breast cancer) within 10 years of diagnosis, in people who will be taking hormone therapy for at least five years.
2. Who is Oncotype DX for?
The test is suitable for people recently diagnosed with early stage invasive breast cancer that:
- Has not spread to the lymph nodes under the arm
- Is oestrogen receptor positive (ER+)
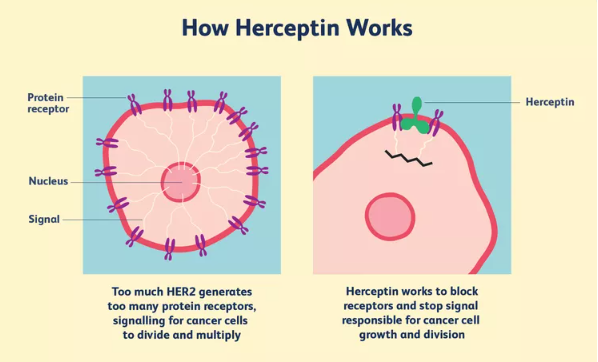
- Is HER2 negative (HER2-)
Sometimes the test may be considered for people whose breast cancer affects one to three lymph nodes under the arm.
The test is not suitable for people whose breast cancer is oestrogen receptor negative or HER2 positive.
3. Why is it used?
Your specialist may recommend the Oncotype DX test if the benefit of chemotherapy for you is less clear.
Chemotherapy may be given after surgery to reduce the risk of breast cancer coming back in future.
Whether you’re offered chemotherapy depends on a number of features of your breast cancer. These include:
- The size and grade of the cancer
- Whether it has spread to any of the lymph nodes under the arm
- Whether the cancer is hormone receptor and HER2 positive or negative
For some people the benefit of chemotherapy is clear, but for others it’s less clear.
4. How does it work?
The test is done on a small amount of breast cancer tissue already removed (for example during a core biopsy or surgery).
The tissue is sent to a laboratory in the USA, where the test is carried out. The test looks at groups of genes found in breast cancer.
The results are given separately from your pathology report and are sent to your specialist within 10 to 14 days.
If your specialist has recommended you have hormone therapy before surgery, the test must be done on the tissue removed by a core biopsy, before you start hormone therapy.
5. Oncotype DX score
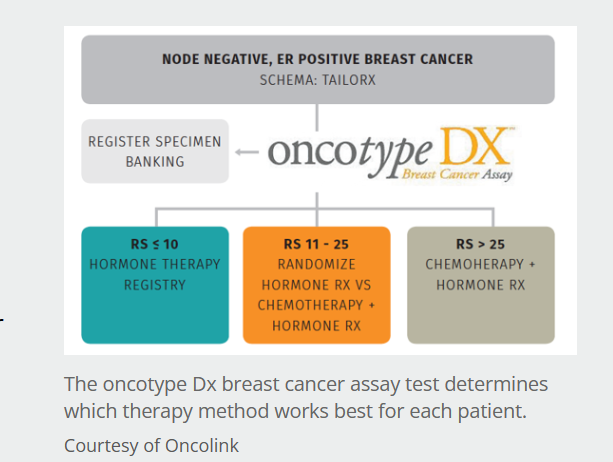
The test gives a score, known as a Recurrence Score, from 0 to 100.
The higher the score, the more likely breast cancer is to come back and the more likely you are to benefit from having chemotherapy as well as hormone therapy.
Your specialist will use the score, along with other information about your breast cancer, to help decide whether chemotherapy would benefit you.
Women over the age of 50
For women over 50:
- A score of 0–25 means you’re unlikely to benefit from having chemotherapy in addition to hormone therapy
- A score of 26 or above means you’re likely to benefit from having chemotherapy in addition to hormone therapy
Women aged 50 or younger
For women aged 50 or under:
- A score of 0–15 means you’re unlikely to benefit from having chemotherapy in addition to hormone therapy
- A score of 16 or above means your specialist will discuss your test result with you to help decide if you’re likely to benefit from chemotherapy
6. Availability and cost
If you don’t have any lymph nodes that contain cancer
If you don’t have any positive lymph nodes, Oncotype DX is available on the NHS across the UK.
If you have between 1 and 3 lymph nodes that contain cancer
If you have between 1 and 3 positive lymph nodes, you may sometimes be able to have the Oncotype DX test on the NHS. Check with your treatment team.
Most private healthcare companies will also cover the cost of the test.
You can also pay for the test yourself, but your treatment team will need to order the test for you and will be sent the results to discuss with you. It costs around £3,000.
7. Oncotype DX Breast DCIS Score test
There’s a specific Oncotype DX test for people with ductal carcinoma in situ (DCIS) who have had breast-conserving surgery (also known as wide local excision or lumpectomy).
Oncotype DX for DCIS can predict the risk of the cancer coming back after surgery. The results of this test may help you and your treatment team decide whether you’re likely to benefit from radiotherapy.
It’s not routinely used on the NHS as there’s less evidence of its benefits for people with DCIS. Some private healthcare providers may cover the cost and you can also pay for the test yourself. For more information, talk to your treatment team.