Short reviews of about he study notes on Vitamins
Fat soluble Vitamins
- Vitamin A – Vitamin B Complex
- Vitamin D – Vitamin C Ascorbic acid
- Vitamin E – Vitamin B1 Thiamine
- Vitamin K
Water soluble
- Vitamin B complex
- Vitamin C
Vitamin B complex
- Vitamin B1 Thaimine
- Vitamin B2 Riboflavin
- Vitmin B3 Naicin
- – Vitamin B5 Pantothenic acid
- – Vitamin B6 Pyridoxin
- Vitamin B7 Biotin
- – Vitamin B12 Cobalamin
- – Vitamin B9 Folic acid

Water soluble vitamins
Biotin B7
– It acts as coenzyme for
- pyruvate carboxylase gluconeogenesisFat Soluble. Vitamins. A, D, E, K. B complex, C. Water Soluble. Vitamins.
- Acetyl CoA carboxylase fatty acid synthesis
- Propionyl CoA carboxylase
Deficiency:
- excessive consumption of RAW eggs
Clinical Features:
- Alopecia
- bowel inflammation
- muscle pain
Vitamin B2
Functions: It acts as coenzyme for pyruvate dehydrogenase — FAD(H2)
Features of deficiency
– Corneal neovascularization
– Cheilosis (cracking and scaling of Lip borders and corners of mouth)
– Magenta colored tongue
* B2 deficiency will cause decrease in ATP
Thiamine Vitamin B1
Functions:
- It acts as coenzyme for pyruvate dehydrogenase
Pyruvate Acetyl CoA
∞ ketoglutarate dehydrogenase
Dehydrogenases are involved in ATP production.
- Maintenance of memory pathway.
Deficiency is due to
- Alcoholism (it interferes with absorption)
- Eating polished rice
Clinical Features:
- Amnesia
- Lactic acidosis
Normally pyruvate converts into acetyl CoA but in B1 deficiency it will convert into lactic acid.
- Wernicke’s encephalopathy
- Ataxia
- Nystagmus
- Ophthalmoplegia
- Korsakoff syndrome
- Confabulation (imagined memory, informal conversation)
- Psychosis (loss of contact with reality)
B1 deficiency destroys mammillary bodies associated with memory.
In a Hypoglycemic patient, first infuse vitamin B1 if he is alcoholic.
- White Beri-Beri
High cardiac output will lead to cardiac failure and body becomes edematous.
Niacin Vitamin B3
It is required to make NAD, NADP — Used by dehydrogenases.
Deficiency: is always dietary.
Clinical Features:
- Pellagra (4D)
- Diarrhea
- dementia
- dermatitis
- Death (if not treated)
- Hartnup disease (Genetic disease)
Due to decreased absorption of tryptophan by the Kidneys body fails to retain tryptophan — an essential amino acid required to make Vitamin B3.
– Treat with increased protein diet
Pantothenic acid vitamin B5
Function: Acts as coenzyme for dehydrogenases and synthases.
- Required to make acetyl coenzyme for fatty acid metabolism and TCA cycle.
Deficiency is very rare
but can cause dermatitis, enteritis and alopecia.
Thyroxin Vitamin B6
Function:
- It acts as coenzyme for enzyme of heme biosynthesis (δ aminolevulinate synthase).
- Acts as coenzyme for aminotransferases AST and ALT
- Important for the maintenance of peripheral nerves.
Deficiency:
1) Most common cause is alcoholism
2) Isoniazid therapy for 6 to 12 months.
Isoniazid is very hepatotoxic.
In Liver cirrhosis AST, ALT are increased and Vitamin B6 is decreased.
Clinical Features:
- Sideroblastic anemia
Less heme less hemoglobin small red blood cells (RBCs) microcytic anemia.
As there is no heme production iron is not used iron builds up in bone marrow erythroblast becomes sideroblasts.
- Peripheral neuropathy
- Homocystenemia
- Convulsions
- Cheilosis
Cobalamin B12
Functions:
- Acts as enzyme for homocysteine methyltransferase (this enzyme untraps folate from the storage form to be active.)
- Coenzyme for methylmalonyl CoA mutase
Source of succinyl CoA — so can cause neuropathy.
Deficiency causes:
- Decrease intake in pure vegetarians
- Pernicious anemia (autoimmune disease)
- Right hemi-colectomy
- Crohnn’s disease
- Infection of diphylobothrium latum
Clinical Features:
- Megaloblastic anemia
- Progressive peripheral neuropathy
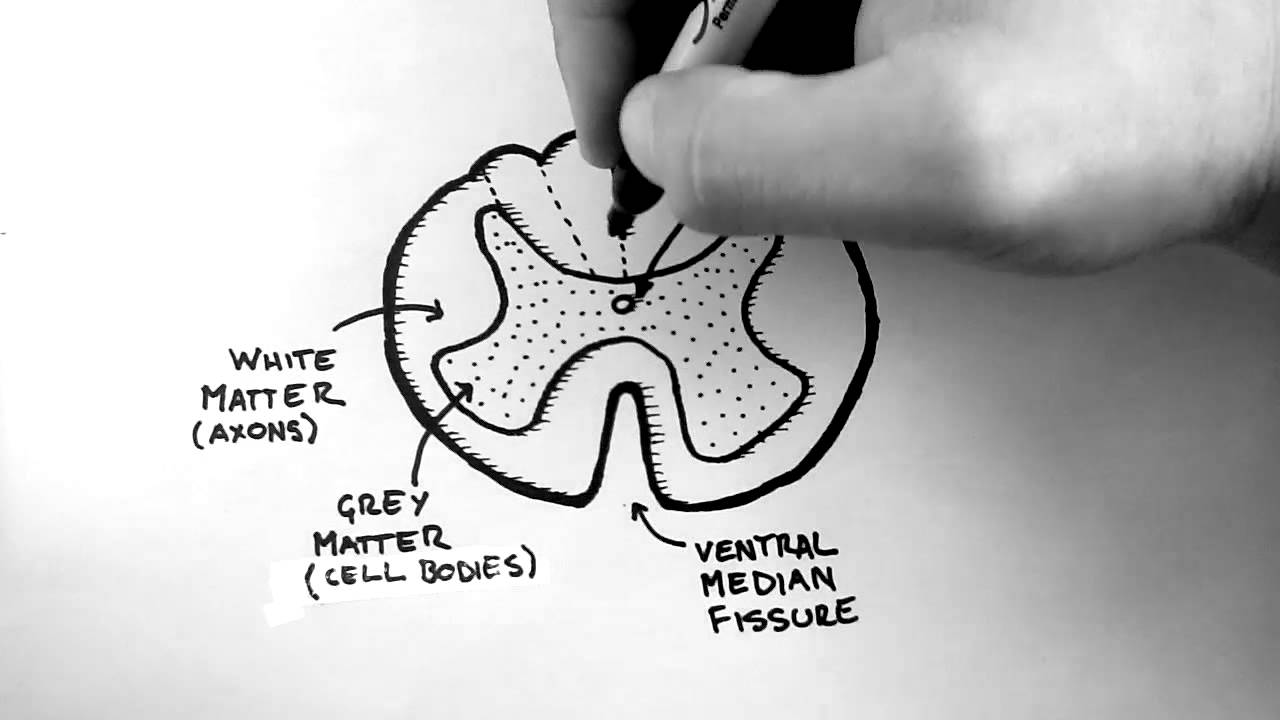
- Sub-acute combined degeneration of spinal cord
- Amnesia
- Fever
- Homocystenemia
Folic acid vitamin B9
Function: It acts as coenzyme for thymidylate synthase.
- Important for biosynthesis of pyrimidine and purine synthesis. So important for RNA and DNA synthesis.
Source is green leafy vegetables.
Deficiency:
- Decrease green leafy food
- Alcoholism
- Pregnancy – in pregnancy, body stores are depleted in 3 months. So patients are advised to take it as tablets.
- Antiepileptic drugs
Clinical Features:
- Megaloblastic anemia
- Neural tube defects — commonly in early pregnancy
Important for the closure of anterior for during first month of gestation. - Homocystenemia
- MI and stroke
Vitamin C: Ascorbic acid
Source: Citrus fruits and green vegetables.
Function: It acts as coenzyme for hydroxylases in pathway of collagen synthesis, Catecholamine synthesis, Responsible for the absorption of iron in stomach.
- Heme of plant Fe+3 with Vit. C will be changed into Fe+2 (which is absorbable)
- Antioxidant nature
Deficiency Clinical Features:
- Weak collagen in blood vessels
- Poor wound healing
- Easy bruising
- Bleeding gums
- Increased bleeding time
- Anemia (platelets binds to collagen through Vitamin C)
– In children - Loss of teeth
- Deformity of Skeleton
- Anemia
- Gum bleeding
Vitamin A
Associated with
- Maintenance of healthy epithelium
- Vision
- Growth
It has three structures
- Retinol
- Retinoic acid – These two are responsible for healthy epithelium
- Retinal – responsible for vision
Vitamin A is stored in liver.
Deficiency clinical features:
- Night blindness
- Xerophthalmia
- Corneal ulceration
- Bitot spots (opaque Spots)
- Alopecia
- Growth retardation – loss of Taste buds – no appetite
- Squamous metaplasia of lungs – recurrent infections
- Vitamin A drugs are used for acne (But these are contraindicated in pregnancy due to systemic absorption)
- Dry scaly skin
- Infertility
- Immune suppression
Vitamin D
Synthesis and activation: Derived from cholesterol
7-dehydrocholesterol
Skin Ultraviolet light on skin
Cholecalciferol (vitamin D3)
Liver
- 25, hydroxylase, 25-hydroxy Cholecalciferol
Kidney –>
- 1α- hydroxylase
- 1, 25 dihydrocholecalciferol (active form)
- Responsible for Ca+ reabsorption to bones.
- Parathyroid hormone – Bones reabsorption of calcium
PTH acts on kidney to retain calcium and excrete phosphorus But GIT doesn’t have reception PTH. - Parathyroid hormone – induce Kidneys – 25-hydroxycholecalciferol to become active – it comes to receptor at GIT to increase calcium reabsorption.
Causes of Vitamin D3:
- Decrease exposure to sunlight
- Liver failure and cirrhosis
- Renal failure
- Decrease intake of vitamin D (fortified food)
- Malabsorption
Dietary source:
- Saltwater fish
- egg yolks
- Supplemented in many products like milk, yoghurt and cereals.
Functions of vitamin D:
- Works at GI tract for calcium and phosphorus absorption
- On kidney – reabsorption of calcium
- On bones – new bones formation
- Add calcium to the bones.
Vitamin D deficiency
- Ricketts In children
- Osteomalacia in adults
- Hypocalcaemia, hypophosphatemia
- Bone demineralization
Vitamin D toxicity
- Hypercalcemia – can cause renal failure
- Hyperphosphatemia
Vitamin E (helps for a good pregnancy)
- Known as α-tocopherol
- Acts as an antioxidant
Function
- As lipid soluble vitamin – it protects other lipids from oxidative damage.
g. LDL cholesterol
Deficiency clinical features:
- Hemolytic anemia
- Acanthocytosis
- Peripheral neuropathy
- Ataxia
- Effects dorsal column of spinal cord
Vitamin K
Function:
- Important for Gamma carboxylation of vitamin K dependent clotting factors 2, 7, 9, 10 and anticoagulant protein C and S.
- All these required Ca+ to be active
- Vitamin K binds Calcium to different proteins.
- Used as antidote for warfarin.
Causes of deficiency
- Fat Malabsorption
- Long term antibiotics
- Breast milk
- Anticonvulsant in pregnancy
Clinical Features:
- Bleeding and easy bruising
- Increased PT
- In Warfarin toxicity fresh plasma is given, then vitamin K.
- Hemorrhagic disease – with no connective tissue like Vitamin C.