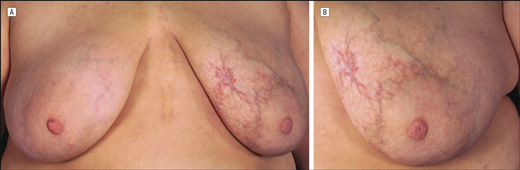
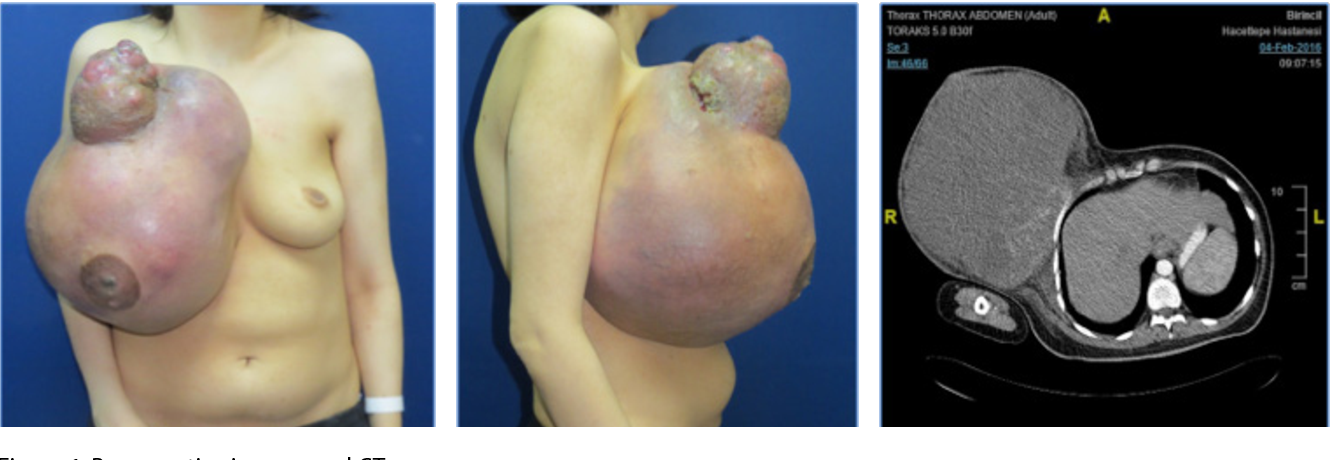
Diffuse dermal angiomatosis is rare and usually considered a variant of reactive angioendotheliomatosis. It generally involves the extremities of patients with severe vascular disease and other comorbidities. Two patients with breast involvement have been described; however, neither had a relevant medical history or a vaso-occlusive disorder, but both had large pendulous breasts, and 1 was positive for IgM anticardiolipin and antinuclear antibodies.
Diffuse dermal angiomatosis (DDA) is a benign, cutaneous vascular disorder. It was first described as a subtype of reactive angioendotheliomatosis (RAE) in 1994 by Krell et al.1 More recently, DDA has been recognized as a distinct, rare variant of RAE associated with smoking, trauma, underlying vaso-occlusion, and hypercoagulability.1–3 Clinically, DDA manifests with tender, violaceous-to-erythematous ulcerated plaques and purpuric papules.1,4 Lesions may also have central ulceration with surrounding tissue necrosis. Lesions tend to persist and progressively enlarge.5–8 While the extremities are the most commonly reported location, there have been several reported cases of DDA of the breast (DDAB), indicating that DDAB is likely more prevalent than previously thought.5,9–13 Herein, we report a case of bilateral DDAB and review the management strategies utilized for this disease to date.
DDA is a unique variant of RAE commonly reported on the lower extremities and, more recently, in women with large, pendulous breasts.1,2 DDAB tends to affect individuals aged 40 to 60 years who have multiple risk factors for atherosclerosis (i.e., hypertension, hyperlipidemia, diabetes mellitus, chronic smoking history, previous heart disease, and stroke).10,13 The differential diagnosis includes acroangiodermatitis, Kaposi sarcoma, and low-grade angiosarcoma. Histologically, a proliferation of endothelial cells and microscopic capillaries in the dermis is seen, in contrast to the intraluminal proliferation of endothelial cells seen in classic RAE.2,14 CD31, CD34, and ERG stains are positive, underscoring benign dermal endothelial cell proliferation. Human herpesvirus 8 testing is negative.3,9,14–16 Although the pathogenesis of DDA remains unclear, it is postulated that angiogenesis is due to up-regulation of vascular endothelial growth factor, secondary to chronic ischemia and hypoxia.4
DDA has been linked to underlying chronic and focal hypoxia secondary to multiple etiologies including severe peripheral vascular disease, subclavian artery stenosis, hypercoagulable states like antiphospholipid syndrome, monoclonal gammopathy, “steal syndrome” from arteriovenous fistula, calciphylaxis, smoking, obesity, and large pendulous breasts (see Table 1).5,7–9,13,16–25 Risk factors shared by most reported patients include large pendulous breasts, elevated body mass index, and smoking history.24 Large, pendulous breasts (which tend to occur along with obesity) are thought to contribute to chronic hypoxia of focal breast tissue via subclinical torsion, compression, repeated micro trauma, and increased pressure.5,9,24 Smoking is known to impair wound healing, with persistent use contributing to atherosclerosis and peripheral arterial disease.10 Severe atherosclerosis can manifest as peripheral arterial disease with occlusion of major vasculature, causing diminished blood flow in the legs and breasts of women.1,9,11,12,17,21,23 As DDA can be an indicator of severe atherosclerosis, patients with relevant risk factors should undergo appropriate workup.
source https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7155956/