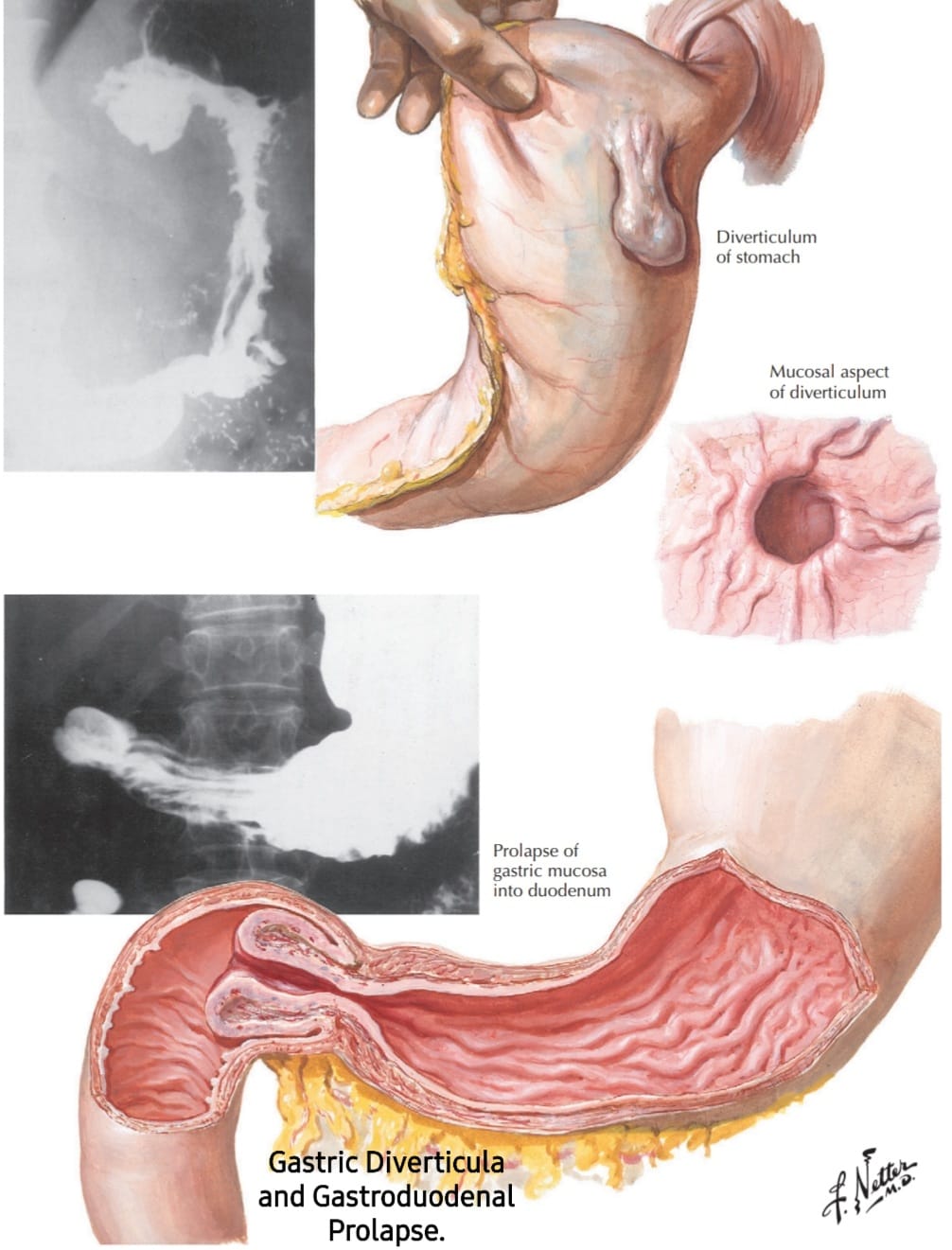
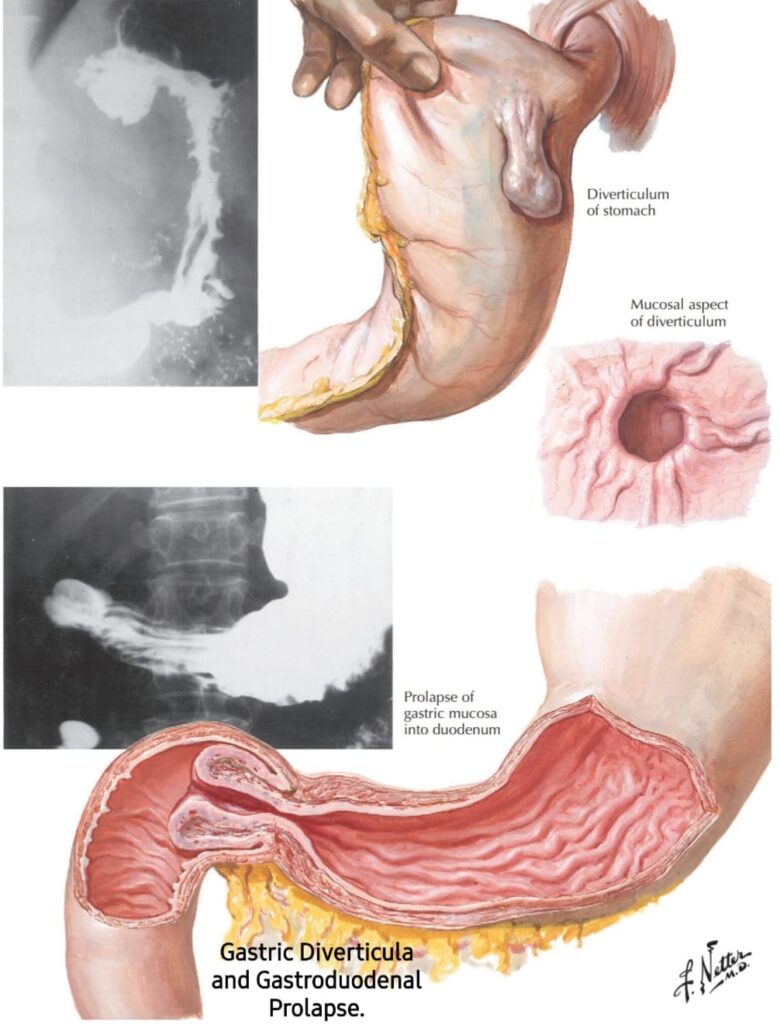
𝗚𝗮𝘀𝘁𝗿𝗶𝗰 𝗱𝗶𝘃𝗲𝗿𝘁𝗶𝗰𝘂𝗹𝗮 are rare and are found in 0.02% of autopsy specimens. Almost all are located on the posterior wall of the cardia and to the left of the esophagus. They are thought to be congenital but occur at the structural weakness of the longitudinal muscles on the posterior surface. Usually, the diverticula contain all layers of the muscle wall and are 2 to 3 cm long and 1.2 cm in diameter. Openings are wide, permit free communication with gastric contents, & may be seen endoscopically. Gastric diverticula are best visualized on a retroflexion view. On barium radiography, they can be missed when the stomach is distended but often are seen on the lesser curvature, and they fi ll and empty regularly.
medicospacecom
•CLINICAL PICTURE:
Diverticula of the stomach are asymptomatic. However, complications have been reported and resulted in resection. Laparoscopic techniques are used effectively to resect the diverticula.
•TREATMENT AND PROGNOSIS:
No treatment is needed for diverticula unless the infrequent complication occurs. When bleeding, perforation from the manipulation, or the rare associated malignancy occurs, resection is performed laparoscopically. Small and most other diverticula are asymptomatic, & prognosis is excellent.
𝗚𝗮𝘀𝘁𝗿𝗼𝗱𝘂𝗼𝗱𝗲𝗻𝗮𝗹 𝗽𝗿𝗼𝗹𝗮𝗽𝘀𝗲:
Prolapse of the gastric mucosa into the duodenum probably results from extreme mobility of the antral mucosa & submucosa. The mucosa of the antrum, which normally is thicker than the mucosa of other parts of the stomach and sometimes assumes a cushion like quality, is pushed through the pyloric ring to lie like a turned-back cuff of a sleeve within the duodenum. Although a fully developed prolapse is rare, partial prolapse is common but of little or no clinical significance.
•Gastroduodenal prolapse is most often a radiologic curiosity, and the duodenal bulb can appear to be filled with a tuberous mass with irregular contours. Diagnosis is easy to make. Occasionally, however, it is difficult to differentiate a prolapse from a polyp or an acute ulcer from marked mucosal edema of the surrounding area. Endoscopists rarely report gastroduodenal prolapse.
•The literature contains a report of a rare episode of strangulation of the mucosa with subsequent signs of pyloric obstruction or gastrointestinal bleeding that required surgical correction.
𝗥𝗲𝗳:Netter’s gastroenterology.