Prostatitis is inflammation of the prostate gland. It is the most common urological problem in men under 50 years old, with an overall prevalence of 2.2-9.7%.
Prostatitis is comprised of acute bacterial prostatitis, chronic bacterial prostatitis, nonbacterial prostatitis, and prostatodynia*.
In this article, we shall predominantly focus on acute bacterial prostatitis, discussing its clinical features, investigations, and management.
*The National Institute of Health classification involves Categories I, II, IIIA, IIIB and IV, all of which near identically correlate to the above classification.
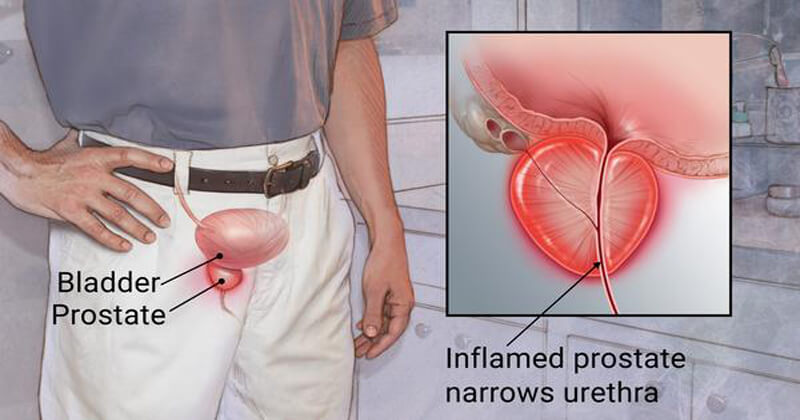
Pathophysiology
Most cases of acute bacterial prostatitis are caused by ascending urethral infection, although occasionally direct or lymphatic spread from the rectum or hematogenous spread via bacterial sepsis can be the cause.
Causative organisms include E. Coli (most common), Enterobacter, Serratia, Pseudomonas, and Proteus species. Sexually transmitted infections, such as Chlamydia or Gonorrhoea, are a rare cause.
Chronic bacterial prostatitis is chronic bacterial infection of the prostate with or without prostatitis symptoms and is thought to be the sequelae of inadequately treated acute prostatitis.
Clinical Features
Acute bacterial prostatitis can present with lower urinary tract symptoms (LUTS), features of systemic infection (including pyrexia), perineal or suprapubic pain, or urethral discharge.
On rectal examination, there is often a very tender and boggy prostate. Associated inguinal lymphadenopathy may also be present.
Chronic prostatitis should be suspected in men who complain of pelvic pain or discomfort for at least 3 months (Prostatodynia), alongside LUTS; the perineum is the most common site for pain, however pain can occur in the suprapubic region, lower back, or rectum.